# Unraveling the Oddities of SARS-CoV-2 and Its Aftermath
Written on
Chapter 1 Understanding the Enigma of COVID-19
Recent studies indicate that the repercussions of COVID-19 are far more peculiar than what one might anticipate from a severe influenza virus.

In the initial phases of the pandemic, prior to our comprehensive understanding of COVID-19, two medical specialties sensed that this virus was unusually alarming. First, pulmonologists observed alarming rates of hypoxemia—low oxygen levels in the bloodstream—and the alarming speed with which previously stable patients deteriorated, necessitating intensive care. The second group, which I also belong to, included nephrologists who noted dysfunctions in dialysis machines. I vividly recall attending to patients undergoing dialysis for kidney failure amid severe COVID infections, witnessing clots rapidly obstructing the dialysis filters. Some patients struggled to complete their treatments as the filters clogged so quickly.
We recognized that COVID-19 was more deadly than the flu, but these odd manifestations made it clear that it was not merely a particularly severe respiratory illness; it presented a range of effects on the body that we had not encountered before. This curiosity has drawn my attention to studies comparing patient outcomes post-COVID with those following other respiratory infections. This week, we delve into a fascinating study suggesting that COVID-19 may trigger autoimmune disorders such as rheumatoid arthritis, lupus, and vasculitis.

The study under discussion, published in the Annals of Internal Medicine, leverages comprehensive electronic health record systems from South Korea and Japan. This collaboration resulted in an impressive cohort of over 20 million individuals from 2020 to 2021.
The focal point of the study? COVID-19 infection, which affected nearly 5% of this population during the study timeframe. It's worth noting that there was a period when COVID infections were relatively well-controlled, especially in certain regions.

The researchers aimed to evaluate the incidence of autoimmune diseases among those infected with COVID-19 in comparison to two control groups: the general population and individuals infected with influenza. While the first control group provided interesting insights, it posed challenges due to the differences between those infected with COVID and the general populace. The second control group, consisting of flu patients, was more appealing; the similarities in risk factors for both COVID and influenza meant that these individuals were more likely to have received medical care, ensuring they were "within the system."
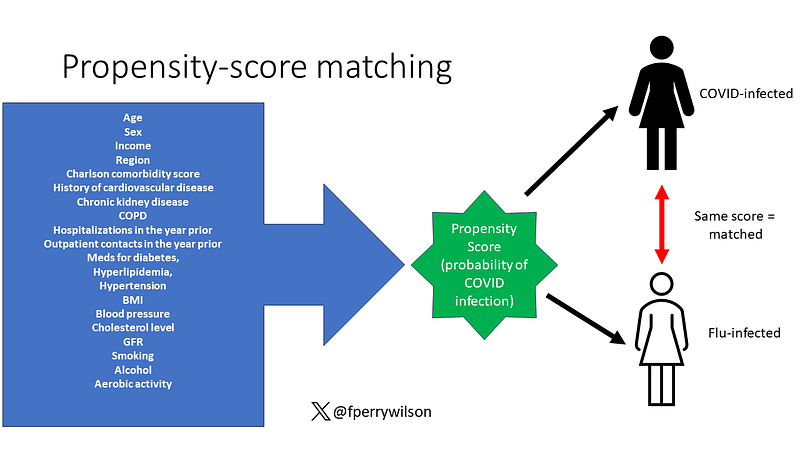
However, merely identifying these individuals was insufficient. The authors employed propensity score matching to pair COVID-infected individuals with similar individuals from the control groups, where one had contracted the virus and the other had not (at least during the study period).
With statistical balancing established, the authors examined the likelihood of various autoimmune disorders. Findings indicated that those who contracted COVID-19 were more susceptible to autoimmune conditions, connective tissue diseases, and inflammatory arthritis, particularly in Japan.

The authors acknowledged that a diagnosis might not equate to the actual presence of a disease. Therefore, they conducted a further analysis focusing solely on individuals who received treatment for autoimmune conditions—revealing even stronger correlations within that group.

The risk appeared to peak within the first six months following COVID-19 infection, suggesting a potential biological mechanism at play wherein the virus may disrupt the immune system.

Interestingly, the risk remained consistent across both COVID variants present during the study. The only factor that mitigated this risk? Vaccination. This finding is particularly noteworthy, as the exposure cohort was defined by prior COVID-19 infection; thus, the protective mechanism is not merely about preventing infection but possibly about preparing the immune system to handle COVID-19 more effectively.

While this study is observational and does not allow for causal inferences, it reinforces my long-standing belief that COVID-19 is indeed an unusual virus—one that manifests effects distinct from the respiratory viruses we have typically encountered. While I cannot definitively claim that COVID-19 induces immune dysfunction leading to autoimmune diseases based on this study, it certainly wouldn't surprise me.
The first video titled "SARS-CoV-2 Is a Very Weird Virus" discusses the unique characteristics of this virus and its implications on health.
The second video titled "COVID-19 is on the rise with wide-ranging symptoms" highlights the diverse symptoms associated with COVID-19 and its current trends.