# Transforming Breath: The Role of Hypoxia in Spinal Cord Recovery
Written on
Chapter 1: Understanding Physical Therapy's Unique Approaches
Physical therapy can sometimes seem unconventional. Therapists often place patients in unusual positions, work on obscure muscle groups, and guide individuals through seemingly simple balance exercises that can be frustratingly difficult, leaving them bewildered as they stumble on a piece of foam. While physical therapy can be a challenging and physically demanding experience, few would anticipate that some treatment regimens involve intentionally reducing a patient’s oxygen supply—yes, you heard that right. This might sound strange, but it’s a method employed to aid recovery from spinal cord injuries.
This method is known as Acute Intermittent Hypoxia (AIH). It is used to assist individuals recovering from severe spinal cord injuries resulting from accidents, violence, or other traumatic events. During AIH, therapists carefully limit a patient’s oxygen intake for brief periods. At first glance, this practice seems counterintuitive—after all, we know that oxygen is essential for life and healing. While hyperbaric oxygen therapy is beneficial for treating various injuries, AIH takes a completely different approach. So, how does reducing oxygen levels promote healing? To grasp this concept, let’s explore a familiar experience.
Consider weightlifting: if done correctly, it can be painful but rewarding. As you squat or lift weights, your muscles endure discomfort from lactic acid build-up, yet this struggle is essential for growth. Each workout creates tiny tears in your muscles, tendons, and bones. Despite being taxing, this process is vital for development. After a workout, the body enters recovery mode, repairing the damage and coming back stronger. The principle is straightforward: stress is necessary for strength to follow.
While the recovery process may seem automatic, it involves a complex interaction of hormones and chemicals that signal the body to heal. This signaling mechanism is vital for recovery, and while it may be intricate, it’s crucial to understand that it exists. This repair cycle is more nuanced than it may initially appear.
AIH mimics this workout dynamic: it applies stress to the body, prompting a breakdown that leads to hormonal and chemical responses, ultimately resulting in enhanced healing. However, unlike traditional exercise where specific muscles rebuild, AIH impacts the respiratory system—yet the benefits extend far beyond that.
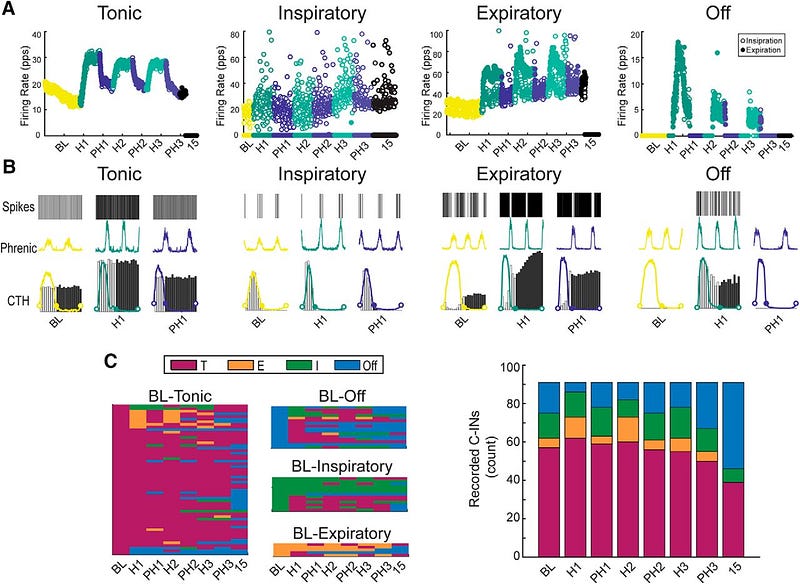
The body contains specialized cells called chemoreceptors, located in the carotid arteries, which detect low oxygen levels (hypoxemia). These cells are primarily inactive during normal oxygen states. However, when oxygen levels drop—such as during AIH—these chemoreceptors react and initiate a cascade of chemical signals. Similar to muscle cells responding to damage, chemoreceptors release chemicals that influence the entire body. Instead of localized responses, these signals can produce far-reaching effects that are particularly beneficial for those with spinal cord injuries.
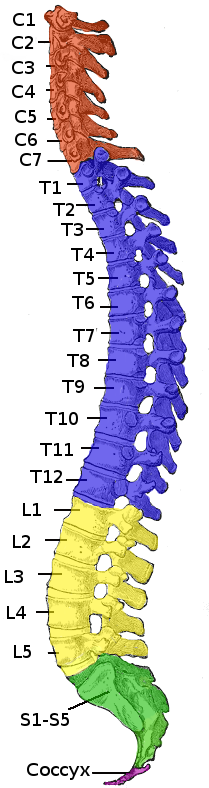
The impact of spinal cord injuries can vary greatly depending on the injury's location. For instance, an injury at L3 may result in a loss of knee extension while preserving hip function, whereas injuries at C3 or C4 can necessitate life support. Notably, over 60% of spinal cord injuries are incomplete, meaning some neural connections remain intact. These patients often face significant challenges during rehabilitation, as regaining functionality can take extensive therapy and time. The process of neuronal healing and adaptation, known as long-term facilitation (LTF), is critical yet time-consuming. Furthermore, some individuals exhibit slower recovery rates due to less adaptable neurons.
AIH shows promise in enhancing healing among individuals with less plastic neurons by improving metaplasticity—the ability of neurons to adapt and recover. This occurs through a fascinating mechanism: chemoreceptors send broad signals across the body, starting with serotonin, which eventually leads to the release of Brain-Derived Neurotrophic Factor (BDNF).
BDNF plays a crucial role in neuronal growth and development, guiding the formation of new neurons, promoting connections, and synchronizing neural activity. In individuals with spinal cord injuries, reconnecting neurons is vital for recovery, and BDNF accelerates this process significantly.
As this research area evolves, it holds the potential to transform spinal cord injury treatments. Ongoing clinical trials are yielding promising results, demonstrating that combining AIH with traditional therapy can lead to quicker recovery. Remarkably, just 30 minutes of AIH-assisted therapy can be as effective as six hours of standard physical therapy.
As we conclude, you might wonder how this information is applicable to you. While you may not directly benefit from AIH, especially if you're fortunate enough to avoid spinal cord injuries, there are valuable takeaways. First, physical therapists are continually innovating and improving treatment methodologies, profoundly impacting countless lives each year. Second, if you wish to support this field, consider contributing to the Foundation for Physical Therapy Research, which focuses on advancing PT research to foster a healthier world and has been funding AIH studies for years.
In summary, administering intermittent hypoxia in a controlled manner can be a pivotal factor in healing and enhancing the quality of life for many individuals. The future of this therapeutic approach looks promising, and the results may soon be seen on a global scale.
Chapter 2: The Science Behind Intermittent Hypoxia
Explore the connection between intermittent hypoxia and brain health in this insightful lecture by Dr. Jack Feldman, focusing on its implications for neurological rehabilitation.
Learn how to respond effectively to low oxygen levels and understand hypoxia and cyanosis through this informative video.